Soap Notes For Nurse SOAP Note - What Is It? Healthcare workers use Subjective, Objective, Assessment, and Plan (SOAP) notes to relay helpful and organized information about patients. When everyone in the medical field uses different formats, it gets a tad Psychiatric SOAP Example. psychclerk.bsd.uchicago.edu. S: "I wanted to talk to my kids about how guilty I feel about my ♦ Example: Needs referral to mental health specialist for mental health assessment. ♦ Example.
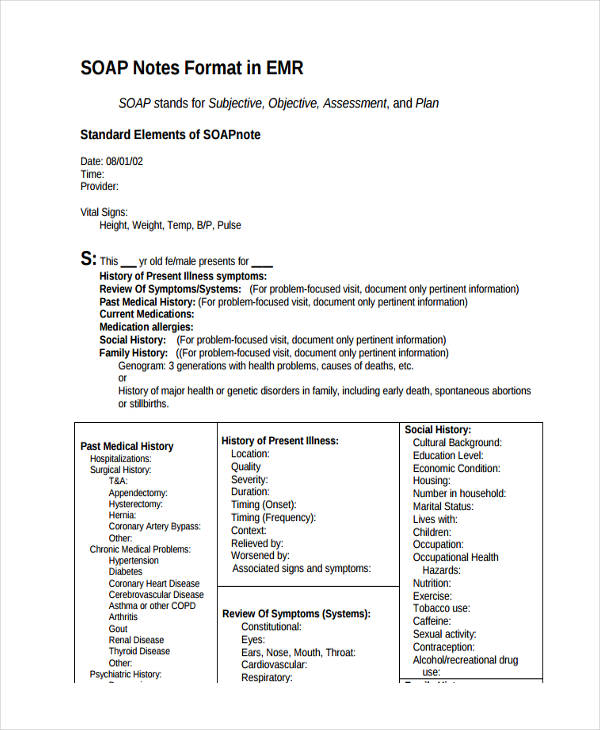
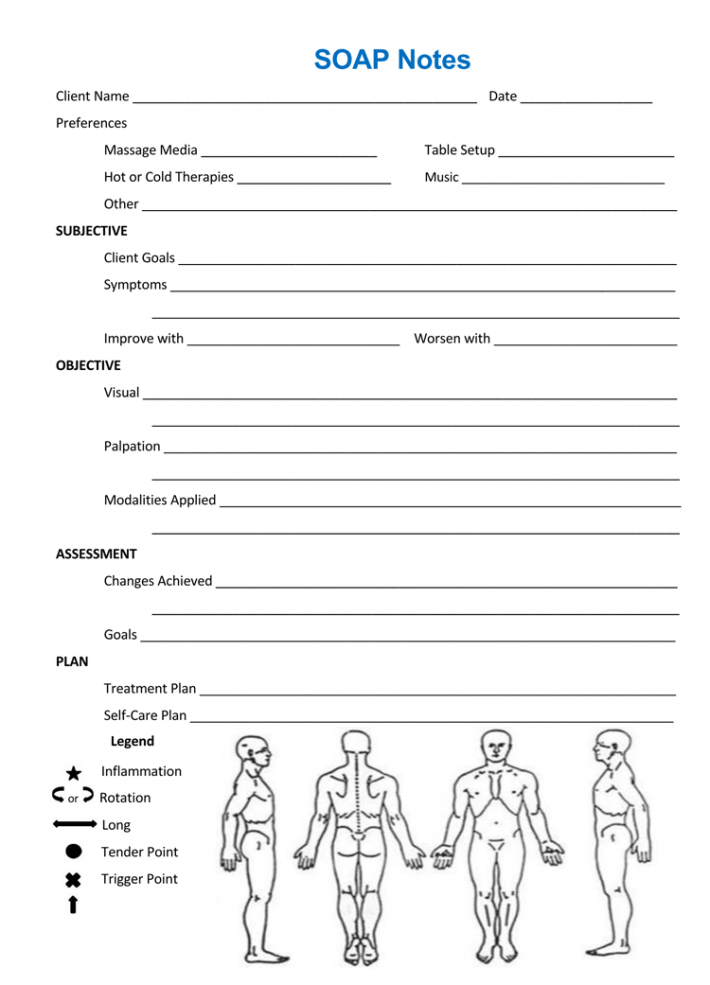
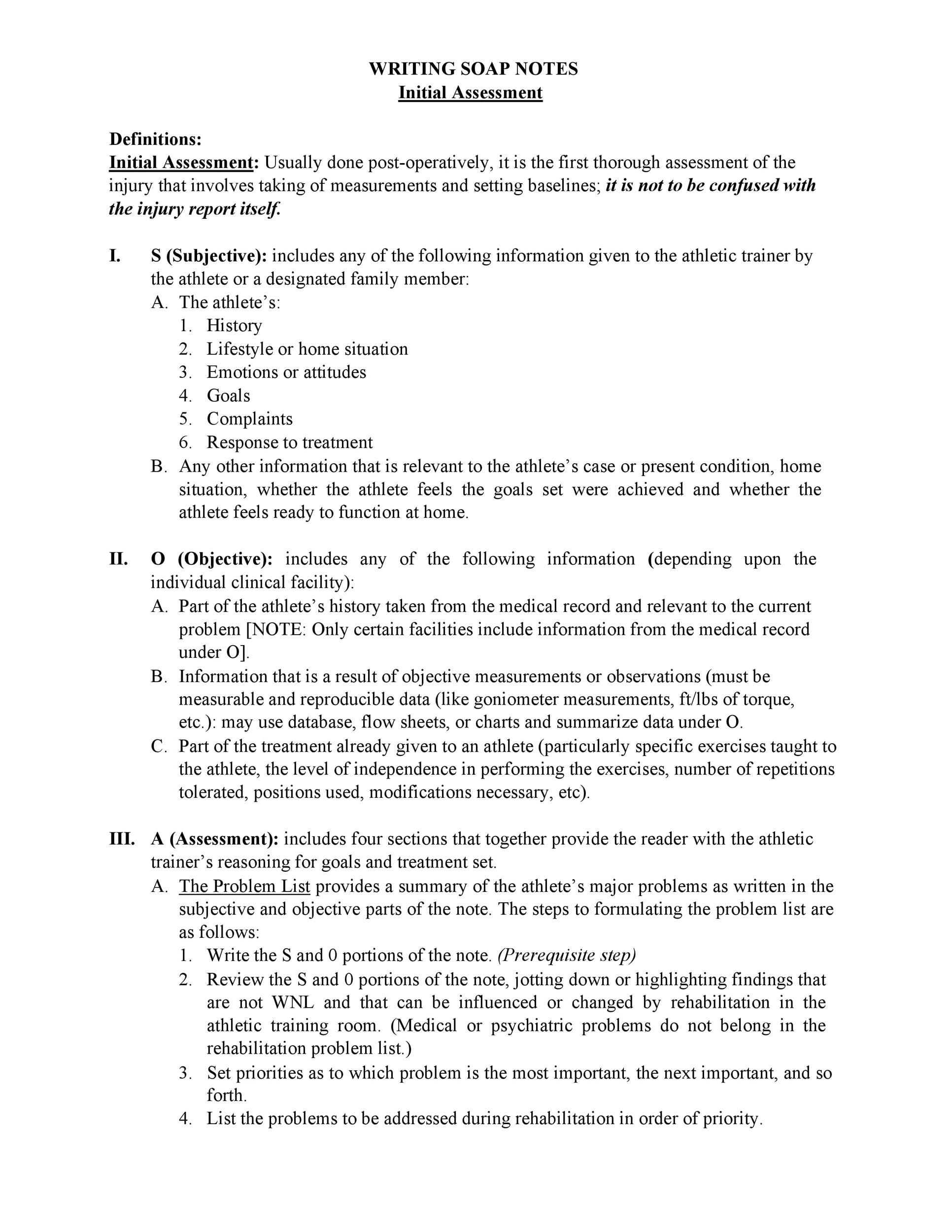
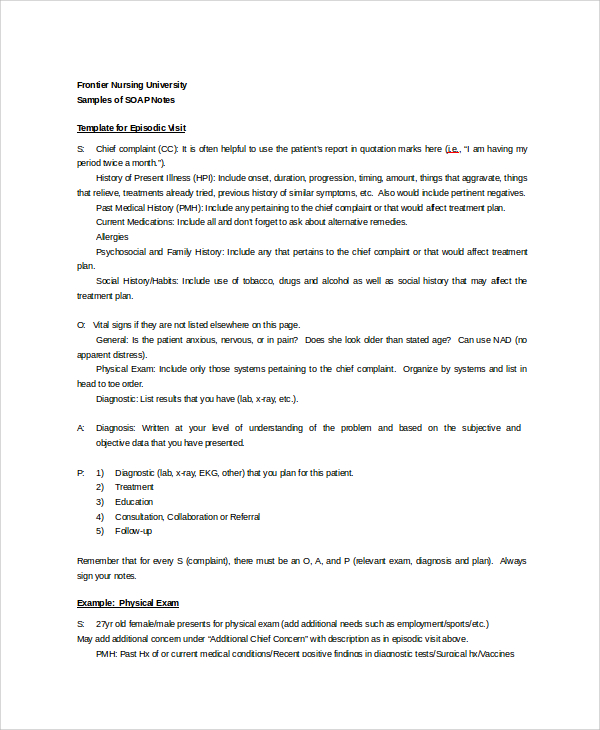
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note.
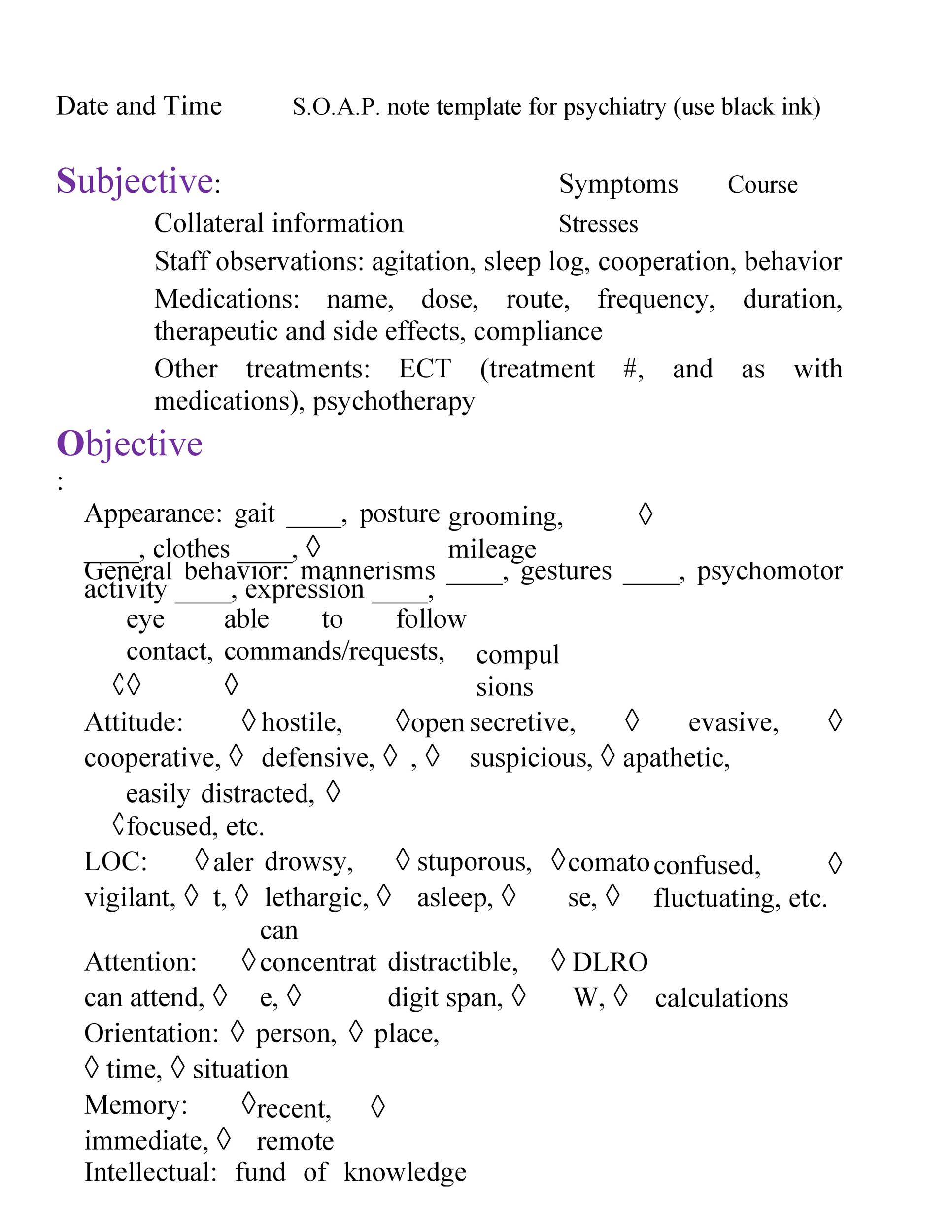
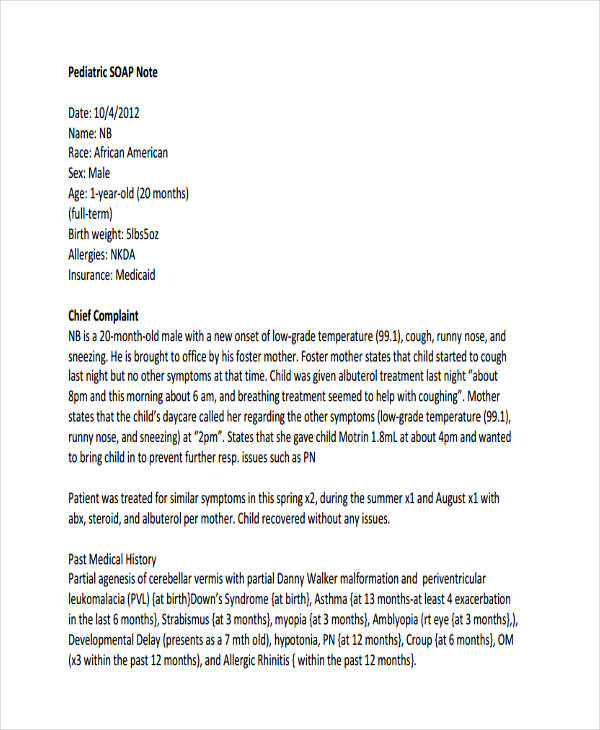
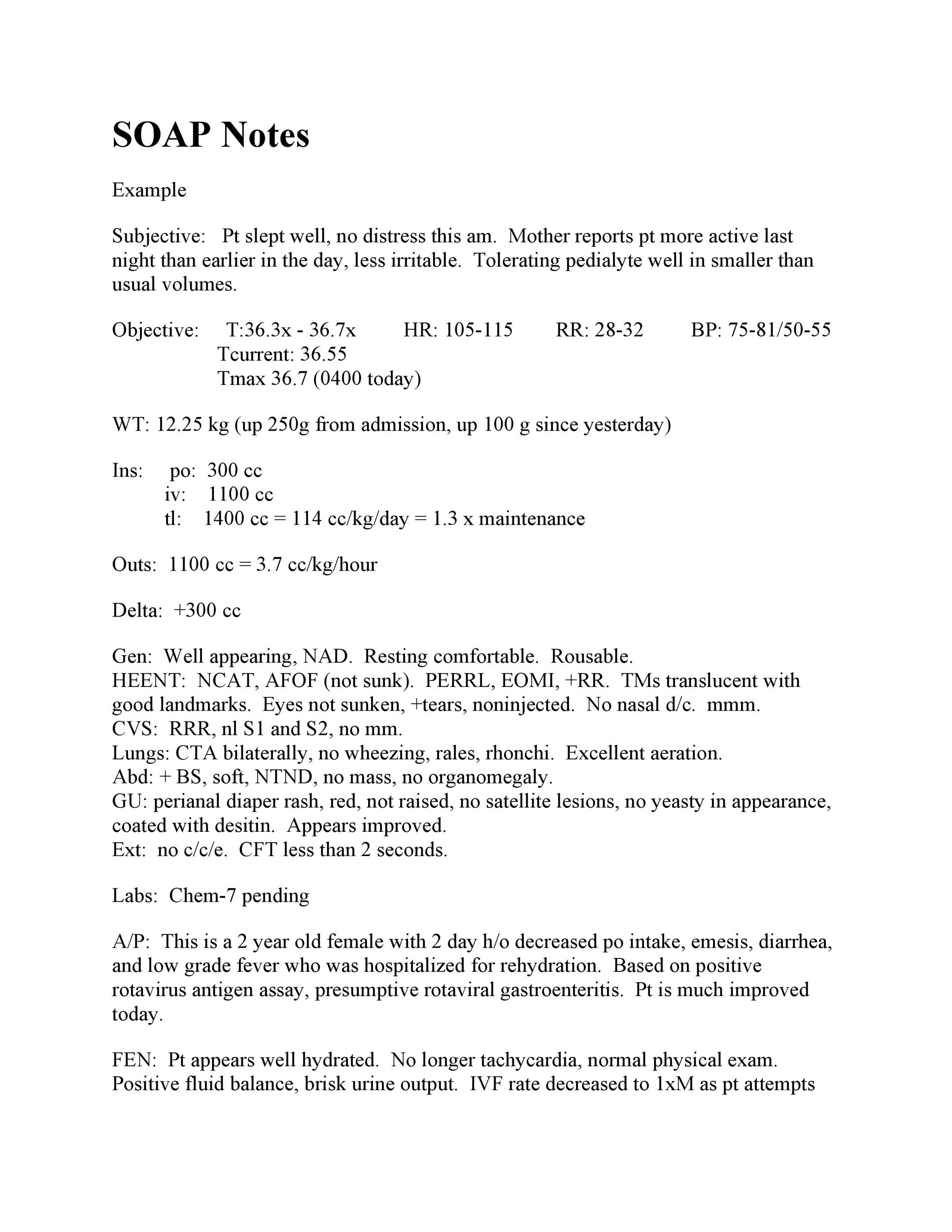
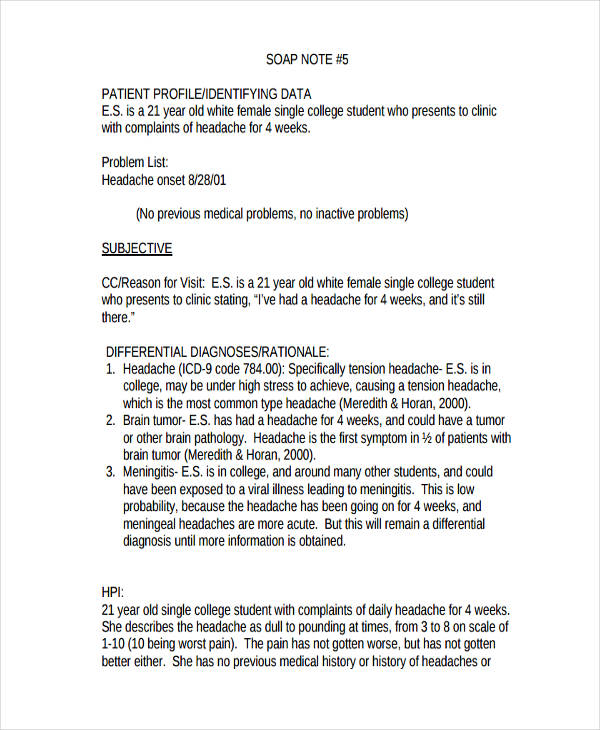
The Soap Note Examples are used widely by medical professionals such as doctors and nurses for listing down all their findings regarding the health condition of their patients. Top Contributors - Rachael Lowe, Scott Buxton and Kim Jackson. Table of Contents How to Write SOAP Notes SOAP Note Examples for Mental Health SOAP Note Example: S: The patient states that she has not been able to use her wheelchair around her home due to her "hands hurting" and "I am not able to get a good grip." Infant soap note example PDF template free download.
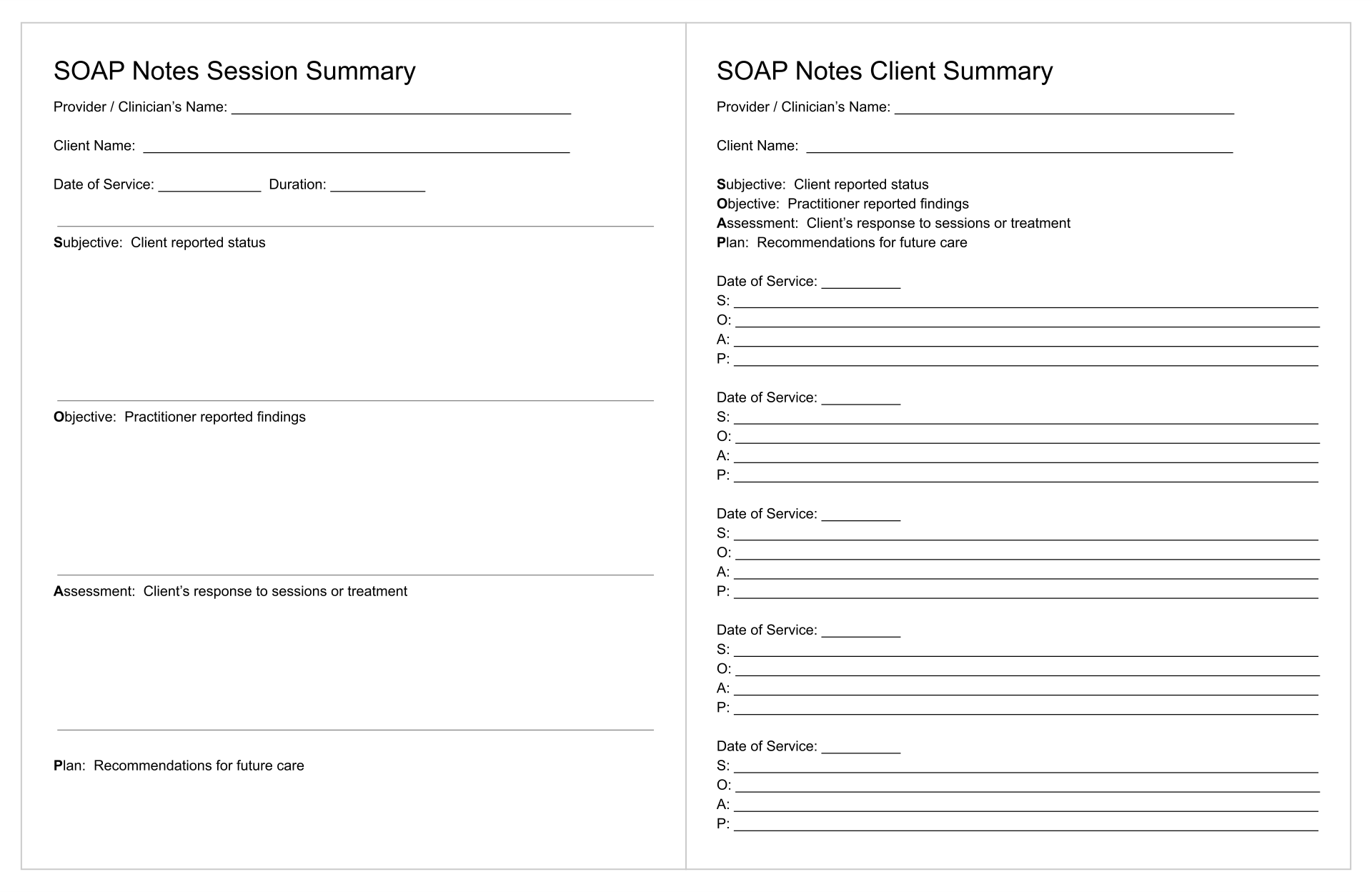
A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the Every medical institution needs to have a SOAP note example or template because it is very.
A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the Every medical institution needs to have a SOAP note example or template because it is very.
Healthcare workers use Subjective, Objective, Assessment, and Plan (SOAP) notes to relay helpful and organized information about patients. Soap Note Example CLICK HERE ►► http By the end of this brief presentation on SOAP Note examples you will take away these three things: Understand the SOAP acronym View a practical. SOAP Note Example for Mental Health Care Professionals. Top Contributors - Rachael Lowe, Scott Buxton and Kim Jackson. This example shows how SOAP notes differ depending on who's writing them and which stage the patient is at (i.e. initial consultation versus day two of their surgery recovery).
Pertinent review of systems, for example Also see your Bates Guide to Physical Examination for excellent examples of complete H & P and SOAP note formats. The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. The Subjective, Objective, Assessment, and Plan (SOAP) note is a widely used documentation method for healthcare providers. A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the Every medical institution needs to have a SOAP note example or template because it is very.